Rhegmatogenous Retinal Detachment after Cataract or Refractive Lens Extraction
Preface
The whish for spectacle independence, low complication rates and the still improving intraocular lenses have increased the Mondial numbers of cataract extraction and refractive lens exchange. Surgery is done more frequently at a younger age. This has large implications for the posterior segment. We see an increased number of posterior vitreous detachments, disturbing floaters and rhegmatogenous retinal detachments after cataract and refractive lens surgery.
As a cataract and vitreoretinal surgeon, I see many colleagues struggle how to explain the increased rhegmatogenous retinal detachment risk after cataract surgery. From the literature and my more than twenty years of experience as a VR surgeon I made an inventory and summarized RRD risk percentages. With the help of an epidemiologist I tried to make an easy tool which can help surgeons explaining the RRD risk after cataract surgery to their patients.
Frank T Kerkhoff, MD PhD
ophthalmologist, anterior, posterior and refractive surgeon
Go to the Retinal Detachment Calculator
Objective
Educational tool for Cataract and Refractive surgeons to evaluate the Rhegmatogenous Retinal Detachment (RRD) risk in patients for cataract extraction and refractive lens exchange.
Introduction
The risk of retinal detachment is a risk that depends on patient related risk factors such as sex, axial length of the eye and concurred myopia, lattice degeneration, status of the vitreous, the factor age of the patient and the surgical factors such technique of surgery and possible complications.
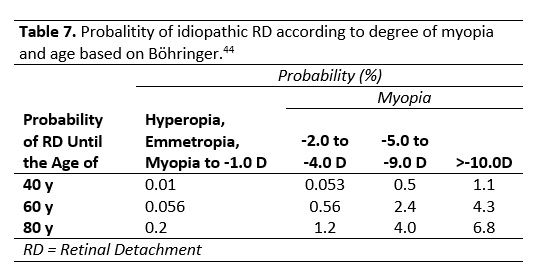
By Böhringer the lifetime risk of RRD constructed assuming a lifespan of 80years. For hyperopia and emmetropia and myopia to -1.0 the risks were 0.2%, myopia from -2.0 to -4.0 1.2%, myopia from -5.0 to -9.0 4% and myopia greater than -9.0 7% (Table 1 Neuhann).
Posterior vitreous detachment
Regmatogenous retinal detachment (RRD) is closely related to a posterior vitreous detachment (PVD). 1 Only small number of RRD are associated without a posterior vitreous detachment. These are the RRD with lattice degeneration and atrophic retinal tears with a detached posterior vitreous that are slowly progressive in young persons. The younger the age of the PVD the higher the chance is of getting a RRD, this because of the larger is the vitreous base (more surface to develop a retinal tear) and the tighter and stronger connections of the vitreous and retina.1
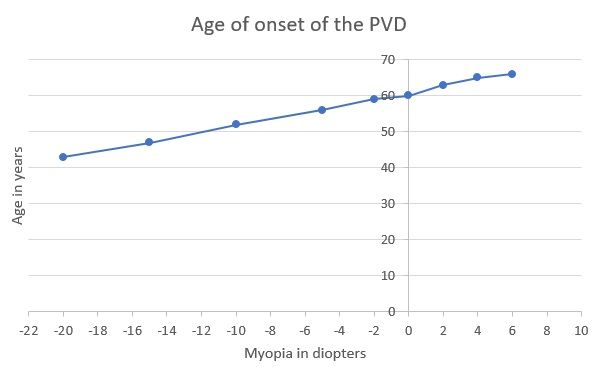
Depending on the myopia (axial length, AL), natural history (eg. intraocular inflammation, trauma, intraocular surgery) the PVD occurs at a certain age. The refractive error and AL are closely related to the age of onset of the PVD. Yonemoto studied the relation between myopia and the age of expected PVD.33 He found a positive correlation between onset age of PVD and refractive error with the regression line:
Y= 0.91 X + 60.93 (Y= age of onset and X refractive error)
Patient with refractive error of +2 diopters:
Y = 0.91x (+2.0) + 60.93 = 63 yrs
Patient with refractive error of -6 diopters:
Y = 0.91x (-6.0) + 60.93 = 55 yrs
Posterior Vitreous Detachment and Lens extraction (cataract extraction or refractive lens exchange)
The most important prognostic factor in lens extraction related RRD is if the posterior vitreous preoperatively is detached or not detached (PVD). The risk of RRD after cataract extraction (CE) in eyes with a posterior vitreous detachment (PVD) preoperatively is 1% and without a preoperative PVD up to 22%.1 So with a PVD prior to the CE decreases the risk of RRD tremendously. Several theories the mechanical and biochemical changes in the vitreous might cause are the PVD induced after a CE. 32-33
Depending on the technique of the cataract surgery and the follow up period the percentage of postoperative PVD changes in different publications. In A small series of non-myopic aphakic patients after lens removal, 50% of eyes developed a PVD.
Mirshahi investigated the PVD frequency in 188 eyes after CE. Of the group 58 eyes (30.9%) had at preoperative examination no echographic signs of a PVD. Of those eyes 24 eyes (41%) had a partial PVD and 10 eyes (17%) a complete PVD within one year. In 28 eyes (82.4%) this occurred within the first month after the surgery reinforcing the association between PVD and CE. Because of the small numbers of eyes determination of risk factors was not possible.32
Ripandelli investigated the PVD and RRD occurrence in 453 emmetropic eyes after cataract extraction with a total follow up time of 5 years. In 188 eyes was at preoperative examination no PVD determined. Of these eyes 78.7% (148/188) developed over time a PVD. They also concluded that although the development of a PVD after CE was not statistically related to age, the RRD developed more frequently in in younger patients. A large percentage (87.23%) of postoperative PVD was detected in eyes peripheral retinal lattice degeneration, suggesting that these peripheral degenerations somehow also influence the development of PVD.
In a study of Hilford was concluded that the frequency of postoperative PVD after CE was significantly higher in eyes with an axial length (AL) of more 25mm than eyes with an AL of less than 25mm.
Hikichi investigated 575 eyes without a PVD after the CE for three years. He found that 30% eyes developed a PVD in 3 years. The postoperative PVD percentages were at 12month postoperative significantly higher in the younger group (6th decade and younger) compared to the older groups. And the higher myopes tend to have a higher incidence of PVD after CE compared to the eyes of other refractive errors.24
Conclusion: RRD after CE higher in patients without prior PVD, CE induces PVD, PVD frequency after CE higher in myopes (AL > 25mm), patients younger of age and in patients with lattice degeneration.
Lattice degeration
Lattice degeneration is a major risk factor for retinal breaks and RRD after CE.7-8 The presence of lattice degenation is in 8-10% of all eyes, its distributed equally in males and females and does not show any racial preference.7-8. Lattice degeneration was detected 8-24% of the myopic eyes and most frequently in the inferior temporal quadrant. Kirker, Byer, Celor
Of all regmatogenous retinal detachments in 20-30% lattice degeneration was present.7-8 The lifetime risk of RRD in patients with myopia and lattice is higher than in myopic patients without lattice degeneration (S-3 to -5 without lattice 1.2%, with lattice 12.1% and S >-5.0 without lattice 2.2% and with lattice 35.9%).6
Celorio found largest prevalence of lattice degeneration moderate high myopia (AL 26-26.7mm, myopia 6.0-8.7diopters). For him this might explain why the most RRD after in these moderate high myopes. Celorlo
Hikichi concluded that eyes with lattice degeneration have a 6.2fold higher risk for the development of retinal breaks after the development of a PVD after CE.
In a series of Ripandelli is the risk of RRD in eyes with a preoperative PVD after cataract extraction 0.94% in eyes without lattice degeneration and 1.88% with lattice degeneration. In eyes without preoperative PVD the RRD risk after CE was 0.70% in eyes without lattice degeneration and 21.27% with lattice degeneration.
Conclusion: Lattice degeneration major risk factor in general for retinal RRD, especially for retinal breaks in postoperative PVD after CE and for RRD in postoperative PVD after CE. The risk of RRD after CE with lattice is a 20 times fold higher than without.
Lensextraction and Rhegmatogenous Retinal Detachment
Many studies have described the relation between RRD and Cataract extraction or Refractive lens exchange. With all the new lenses available (such as Toric, Bifocal and Trifocal lenses) on the market to treat cataract and refractive problems such myopia, hyperopia and presbyopia we tend to perform lens surgery at an earlier age. For that reason, it is important to make for each patient an RRD risk profile for lens extraction (cataract and refractive lens exchange).
The RRD risk profile includes patients age, sex, vitreous status, lattice degeneration, myopia and axial length in combination of an eye in which the ophthalmologist can estimate the risk of vitreous loss during surgery.
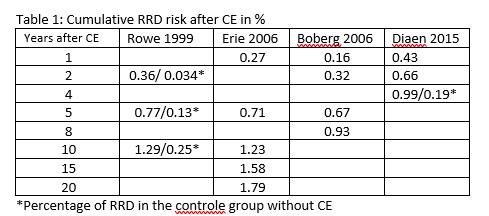
The cumulative RRD risk increase in a patient in different studies up to ten years after the CE. The CE increases the RRD after 10 years in the study of Rowe 5.16times, the more recent study of Diaen showed an increase of 5.2 times even after 4 years.
CE and Myopia
Neuhann studied 2356 eyes with an AL >27mm with a mean age of 64.83±12.47 years after cataract extraction. An RRD developed in 2.2%, of which 70% within 3 years after the surgery.33 This is related to the high incidence of PVD within the first 3 years after cataract surgery.24
Different studies also report an incidence of RRD after CE in eyes with an AL >26 mm of 2.7 (Alio, mean age of 62.22±11.70 years) and 2.8% (Williams mean age of 69.35±11.81 years).3-17
Analysis of AL dependency showed a distinct increase in incidence of 1.6% in eyes with an AL 23-24.9, 8.3% in eyes with an AL of 25-26.9, to 17.1% in eyes of 27-28.9%. The overall incidence of eyes with an AL from 25-28.9 was 10.2%. Laube
Tuft suggest that each mm increase in AL the RRD risk after CE increases with 20%.
CE and age
The study of Alio showed that the <50 years the incidence 1.5 times higher was than the >50 years group. A more recent study of Laube of 13.925 eyes that had cataract extraction in a much younger group (mean age of 51.12±6.78 years) the cumulative RRD risk after 5.7years was 5.5%.
CE and vitreous loss
In the Olmsted study 17% of CE related RRD were associated with vitreous loss during the surgery. A different study showed the increase of RRD after vitreous loss.15-Russel Petrous showed an 13-16-fold increased risk of RRD after vitreous loss. The odds ratio for RRD after a posterior capsular tear was 12.7 in the study of Tuft.
Reference list
-
Agarkar, S., Gokhale, V. V., Raman, R., Bhende, M., Swaminathan, G., & Jain, M. (2018). Incidence, Risk Factors, and Outcomes of Retinal Detachment after Pediatric Cataract Surgery. Ophthalmology, 125(1), 36–42. https://doi.org/10.1016/j.ophtha.2017.07.003
-
Al-Abdullah, A. A., Al-Falah, M. A., Al-Rasheed, S. A., Khandekar, R., Suarez, E., & Arevalo, J. F. (2015). Retinal Complications After Anterior Versus Posterior Chamber Phakic Intraocular Lens Implantation in a Myopic Cohort. Journal of Refractive Surgery, 31(12), 814–819. https://doi.org/10.3928/1081597X-20151111-05
-
Alio, J. L., Ruiz-Moreno, J. M., Shabayek, M. H., Lugo, F. L., & Abd El Rahman, A. M. (2007). The Risk of Retinal Detachment in High Myopia After Small Incision Coaxial Phacoemulsification. American Journal of Ophthalmology, 144(1), 93-98.e2. https://doi.org/10.1016/j.ajo.2007.03.043
-
Bamashmus, M., Al-Salahim, S., Tarish, N., Saleh, M., Mahmoud, H., Elanwar, M., & Awadalla, M. (2013). Posterior vitreous detachment and retinal detachment after implantation of the visian phakic implantable collamer lens. Middle East African Journal of Ophthalmology, 20(4), 327. https://doi.org/10.4103/0974-9233.120019
-
Bokhorst, L. P., & H.C. Zegers, R. (2011). Staarsteek vroeger en nu. NED TIJDSCHR GENEESKD, 155.
-
Burton, T. C. (1998). THE INFLUENCE OF REFRACTIVE ERROR AND LATTICE DEGENERATION ON THE INCIDENCE OF RETINAL DETACHMENT. AM. OPHTH. Soc, LXXXVII.
-
Byer , N. E. (1978). Lattice Degeneration of the Retina. Surv Ophthelmol, 23, 213–248.
-
Byer N.E: Changes in and prognosis of lattice degencration of the retina. Trans Am Acad Ophthalmol Otolaryngol 78:l 14-125, 1974
-
Chandra, A., Banerjee, P., Davis, D., & Charteris, D. (2015). Ethnic variation in rhegmatogenous retinal detachments. Eye, 29(6), 803–807. https://doi.org/10.1038/eye.2015.43
-
Chen, D. Z., Koh, V., Tan, M., Tan, C. S., Nah, G., Shen, L., … Saw, S.-M. (2018). Peripheral retinal changes in highly myopic young Asian eyes. Acta Ophthalmologica, 96(7), e846–e851. https://doi.org/10.1111/aos.13752
-
Chen, S.-N., Lian, I.-B., & Wei, Y.-J. (2015). Epidemiology and clinical characteristics of rhegmatogenous retinal detachment in Taiwan. British Journal of Ophthalmology, 100(9), 1216–1220. https://doi.org/10.1136/bjophthalmol-2015-307481
-
Coppe, A. M., & Lapucci, G. (2008). Posterior vitreous detachment and retinal detachment following cataract extraction. Current Opinion in Ophthalmology, 19, 239–242.
-
Colyear BH: Discussion of Straatsma BR,Allen RA: Lattice degeneration of the retina.
-
Trans Am Acad Ophthalmol Otolaryngol 66:774, 1962
-
Daien, V., Le Pape, A., Heve, D., Carriere, I., & Villain, M. (2015). Incidence, Risk Factors, and Impact of Age on Retinal Detachment after Cataract Surgery in France. Ophthalmology, 122(11), 2179–2185. https://doi.org/10.1016/j.ophtha.2015.07.014
-
Day, A. C., Donachie, P. H. J., Sparrow, J. M., & Johnston, R. L. (2016). United Kingdom National Ophthalmology Database Study of Cataract Surgery. Ophthalmology, 123(8), 1711–1715. https://doi.org/10.1016/j.ophtha.2016.04.002
-
De la Huerta, I., & Williams, G. A. (2018). Rhegmatogenous Retinal Detachment after Pediatric Cataract Surgery. Ophthalmology, 125(1), 4–5. https://doi.org/10.1016/j.ophtha.2017.08.032
-
Dumas J, Schepens CL: Chorioretinal lesionspredisposing to retinal breaks. Am J Ophthalmol 6l:620-630, l966
-
Erie , J. C., Raecker , M. E., Baratz, K. H., Schleck, C. D., & Robertson, D. M. (2006). RISK OF RETINAL DETACHMENT AFTER CATARACT EXTRACTION, 1980-2004: A POPULATIONBASED STUDY. Trans Am Ophthalmol Soc, 104, 169–175.
-
Gavrilov, J.-C., Gaujoux, T., Sellam, M., Laroche, L., & Borderie, V. (2011). Occurrence of posterior vitreous detachment after femtosecond laser in situ keratomileusis: Ultrasound evaluation. Journal of Cataract & Refractive Surgery, 37(7), 1300–1304. https://doi.org/10.1016/j.jcrs.2011.01.022
-
Gray, R. H., Evans, A. R., Constable, I. J., & McAllister, I. L. (1989). Retinal detachment and its relation to cataract surgery. British Journal of Ophthalmology, 73(10), 775–780. https://doi.org/10.1136/bjo.73.10.775
-
GRAY, R. H., EVANS, A. R., CONSTABLE, I. J., & McALLISTER, I. L. (1989). Retinal detachment and its relation to cataract surgery. British Journal of Ophthalmology, 73, 775–780.
-
Graether JM: Retinal changes in degenerative myopia. lnt Ophthalmol Ctin 2:109-132, 1962
-
Hikichi, T. (2012). Time Course of Development of Posterior Vitreous Detachments after Phacoemulsification Surgery. Ophthalmology, 119(10), 2102–2107. https://doi.org/10.1016/j.ophtha.2012.03.050
-
Hilford, D., Hilford, M., Mathew, A., & Polkinghorne, P. J. (2008). Posterior vitreous detachment following cataract surgery. Eye, 23(6), 1388–1392. https://doi.org/10.1038/eye.2008.273
-
Ivastinovic, D., Schwab, C., Borkenstein, A., Lackner, E.-M., Wedrich, A., & Velikay-Parel, M. (2012). Evolution of Early Changes at the Vitreoretinal Interface After Cataract Surgery Determined by Optical Coherence Tomography and Ultrasonography. American Journal of Ophthalmology, 153(4), 705–709. https://doi.org/10.1016/j.ajo.2011.09.009
-
Jiang, T., Chang, Q., Wang, X., & Huang, X. (2012a). Retinal detachment after phakic intraocular lens implantation in severe myopic eyes. Graefe’s Archive for Clinical and Experimental Ophthalmology, 250(12), 1725–1730. https://doi.org/10.1007/s00417-012-2002-z
-
Kang, H. M., Lee, C. S., Park, H. J., Lee, K. H., Byeon, S. H., Koh, H. J., & Lee, S. C. (2014). Characteristics of Rhegmatogenous Retinal Detachment After Refractive Surgery: Comparison With Myopic Eyes With Retinal Detachment. American Journal of Ophthalmology, 157(3), 666-672.e2. https://doi.org/10.1016/j.ajo.2013.12.004
-
MARTINEZCASTILLO, V., BOIXADERA, A., VERDUGO, A., ELIES, D., CORET, A., & GARCIAARUMI, J. (2005a). Rhegmatogenous Retinal Detachment in Phakic Eyes After Posterior Chamber Phakic Intraocular Lens Implantation for Severe Myopia. Ophthalmology, 112(4), 580-585.e1. https://doi.org/10.1016/j.ophtha.2004.09.025
-
Michaelson IC: Retinal detachment: Clinical evidence of the role of the choroid. Acta XVII Concilium Ophthalmologicum, 1954, pp 392-403
-
Mirshahi, A., Hoehn, F., Lorenz, K., & Hattenbach, L.-O. (2009). Incidence of posterior vitreous detachment after cataract surgery. Journal of Cataract & Refractive Surgery, 35(6), 987–991. https://doi.org/10.1016/j.jcrs.2009.02.016
-
MITRY, D., FLECK, B. W., WRIGHT, A. F., CAMPBELL, H., & CHARTERIS, D. G. (2010). PATHOGENESIS OF RHEGMATOGENOUS RETINAL DETACHMENT Predisposing Anatomy and Cell Biology. RETINA, 30, 1561–1572.
-
Neuhann, I. M., Neuhann, T. F., Heimann, H., Schmickler, S., Ger, R. H., & Foerster, M. H. (2008). Retinal detachment after phacoemulsification in high myopia: Analysis of 2356 cases. J Cataract nefract Surg, 34, 1644–1657. https://doi.org/;34:
-
NUZZI, G., & CANTÙ, C. (2002). Vitreous hemorrhage following phakic anterior chamber intraocular lens implantation in severe myopia. Eur J Ophthalmol, 12, 69–72.
-
Panozzo , G., & Parolini, B. (2001). Relationships between vitreoretinal and refractive surgery. opthalmology, 108, 1663–1670.
-
Park, S. W., Lee, J. J., & Lee, J. E. (2018). Scleral buckling in the management of rhegmatogenous retinal detachment: patient selection and perspectives. Clinical Ophthalmology, 12, 1605–1615.
-
Petousis, V., Sallam, A. A., Haynes, R. J., Patel, C. K., Tyagi, A. K., Kirkpatrick, J. N., & Johnston, R. L. (2016a). Risk factors for retinal detachment following cataract surgery: the impact of posterior capsular rupture. British Journal of Ophthalmology, 100(11), 1461–1465. https://doi.org/10.1136/bjophthalmol-2015-307729
-
Ripandelli, G., Coppé, A. M., Parisi, V., Olzi, D., Scassa, C., Chiaravalloti, A., & Stirpe, M. (2007a). Posterior Vitreous Detachment and Retinal Detachment after Cataract Surgery. Ophthalmology, 114(4), 692–697. https://doi.org/10.1016/j.ophtha.2006.08.045.
-
Ruiz-Moreno , J., Montero , J., de la Vega , C., Alió, J., & Zapater , P. (2006). Retinal detachment in myopic eyes after phakic intraocular lens implantation. Journal of refractive surgery, 22(3), 247–252.
-
RUIZ-MORENO, J. M., ALIÓ, J. L., PÉREZ-SANTONJA, J. J., & DE LA HOZ, F. (1999). Retinal Detachment in Phakic Eyes With Anterior Chamber Intraocular Lenses to Correct Severe Myopia. Am J Ophthalmol, 127, 270–275.
-
Sheu , S.-J., Ger , L.-P., & Chen , J.-F. (2006). Axial myopia is an extremely significant risk for young-aged pseudophakic retinal detachment in Taiwan. Retina, 26(3), 322–327.
-
Straatsma BR, Allen RA: Lattice degeneration of the retina. Trans Am Acad Ophthalmol & Otolaryngol 66:600-613, 1962
-
Tassignon, M.-J., Van den Heurck, J. J. I., Boven, K. B. M., Van Looveren, J., Wouters, K., Bali, E., … Mathysen, D. G. P. (2015). Incidence of rhegmatogenous retinal detachment after bag-in-the-lens intraocular lens implantation. Journal of Cataract & Refractive Surgery, 41(11), 2430–2437. https://doi.org/10.1016/j.jcrs.2015.05.026
-
Van de Put, M. A. J., Hooymans, J. M. M., & Los, L. I. (2013). The Incidence of Rhegmatogenous Retinal Detachment in The Netherlands. Ophthalmology, 120(3), 616–622. https://doi.org/10.1016/j.ophtha.2012.09.001
-
Wilkinson , C., Anderson , L., & Little , J. (1978). Retinal detachment following phacoemulsification. Ophthalmology, 85(2), 151–156.
-
Yonemoto , J., Ideta , H., Sasaki, K., Tanaka , S., Hirose , A., & Oka , C. (1994). The age of oneset of posterior vitreous detachment. Graefe’s Arch Clin Exp ophthalmol, 232, 67–70.
-
Zaldivar , R., Davidorf , J., & Oscherow , S. (1998). Posterior Chamber Phakic lntraocular Lens for Myopia of -8 to -19 Diopters. Journal of Refractive Surgery, 14, 294–305. https://doi.org/Postefior Ghamber Phakic lntraocular Lens fot Myop¡a of ’8 to ’11 Diopters